Suppose a man takes a drug to keep his hair. Suppose the drug, approved decades ago by the FDA and marketed under a respectable brand name, causes him to suffer cognitive dysfunction, sexual dysfunction, and neurological deterioration. Suppose these effects were not clearly listed on the label, were unknown to many prescribing clinicians, and were downplayed by the company that distributed the drug. Further suppose that the story of this man, and many others like him, is covered in careful, probing detail by a major news outlet, complete with first-hand interviews, medical records, and a balanced discussion of clinical trial limitations. Now ask yourself: would the same outlet apply this level of scrutiny to vaccines?
If the drug in question is finasteride, and the outlet is The Wall Street Journal’s podcast The Journal, the answer is yes. In an episode titled "A Quick Fix for Hair Loss Is Making Some Men Sick," reporter Kate Linebaugh and her colleague Rolfe Winkler offer a thorough and, at times, harrowing portrait of young men suffering lasting damage after taking the drug for cosmetic reasons. They interrogate clinical trial methods, marketing practices, and regulatory oversight with admirable precision.
The same cannot be said for vaccines.
The paradox is not epistemic, it is cultural. What explains the asymmetry is not the evidence, but the narrative framing that dominates our medical discourse. Ordinary pharmaceuticals, even when prescribed by doctors and approved by regulatory authorities, are fair game for skepticism. But vaccines, especially those administered at scale and under the banner of public health, have acquired a kind of moral invincibility. Critique is construed as heresy.
Begin with methodology. As Winkler notes, many of finasteride’s most troubling effects, panic attacks, suicidal ideation, muscle atrophy, cognitive decline, were either missed or discounted in the drug’s original clinical trials. One endocrinologist interviewed suggests the trials were too short, too small, and too narrowly focused to detect longer-term or systemic harms. This is a familiar critique of pharmaceutical research. It is also, strangely, a critique that vanishes when the subject turns to vaccines.
Standard drug trials, if conducted properly, are randomized, double-blind, placebo-controlled, and long enough to detect both efficacy and safety issues. Yet most vaccines, particularly those given to children, have not been tested against inert placebos. The CDC’s own documentation confirms this. Of the 72 vaccine doses required under the current childhood immunization schedule, none have undergone the kind of rigorous placebo-controlled pre-licensure trials that would be standard for any other class of pharmaceutical.
Why does this matter? Because when clinical trial data are the sole bulwark against adverse events, the quality of those trials is non-negotiable. A saline placebo trial does not just measure whether a vaccine prevents illness, it measures whether it does so without causing other forms of harm. Without it, we are left comparing one intervention against another, with no true baseline.
The same problem afflicts older vaccines. The hepatitis B vaccine, for instance, was approved in the 1980s based on trials that used another vaccine—not saline—as the control. Ditto for DTP, MMR, and others. These foundational products were never subjected to the testing protocols we now consider the gold standard. The consequences, though rarely discussed in mainstream press, are not theoretical. Vaccine court settlements, while rare, have awarded billions to individuals harmed by vaccines. And yet, these settlements—unlike Winkler’s finasteride exposé—rarely reach the front page.
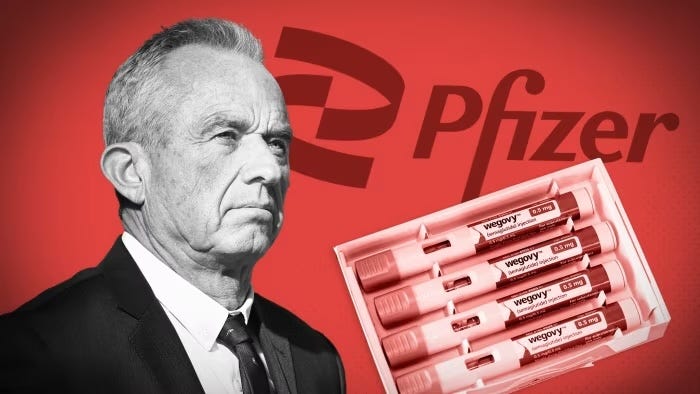
Nor are reporters ignorant of this discrepancy. What explains it is a kind of journalistic bifurcation: skepticism is encouraged when discussing elective drugs like finasteride, but deemed conspiratorial when applied to state-endorsed immunizations. The Journal’s team was able to investigate Hims and Merck without being labeled anti-science. Try the same with Pfizer or Moderna, and the risk is reputational collapse. One is seen as consumer protection, the other as disinformation.
Consider also the marketing channels. Winkler documents how Hims uses a frictionless interface to push young men through a prescription funnel. Ads are tailored to exploit insecurity. Side effects are buried. Yet the mechanism is no different from the CDC’s promotional campaigns during Covid-19. Public health departments created TikTok ads, used influencers, and even partnered with dating apps to encourage vaccination. Unlike Hims, however, the CDC was not required to disclose side effects during these campaigns. The same behavior, depending on the product and the entity behind it, is either condemned or celebrated.
This double standard undermines the principle of informed consent. If young men must be warned of the 1.8% risk of sexual dysfunction from finasteride, should they not also be informed of myocarditis risks from mRNA vaccines? If telehealth firms are faulted for glossing over neurological symptoms, should journalists not also ask why the VAERS system, the CDC’s own adverse event tracker, is never cited in major vaccine reporting? When a drug harms a man’s memory, it makes headlines. When a vaccine harms a child’s heart, it makes a footnote, if that.
It would be easy to say the difference lies in public benefit. Vaccines, after all, are administered not merely to protect the individual but to reduce transmission, to achieve herd immunity. But that argument collapses in the face of recent data. Covid-19 vaccines do not stop transmission. They reduce severity of illness, but the public health rationale for universal vaccination is now more moral than medical. And even if the benefit were uncontested, it would not erase the ethical obligation to disclose risks. The Nuremberg Code did not carve out exemptions for benevolent intentions.
Nor can the media plead ignorance. The very reporters who grilled Merck over finasteride’s post-market data could just as easily have grilled Pfizer over its truncated trials or the FDA over its accelerated approval process. That they did not is not due to lack of skill. It is due to a culture of deference that treats vaccines as sacrosanct.
What explains this? One hypothesis is regulatory capture, but that is too blunt. A better explanation is ideological capture. Vaccines have become a totem of progressive public policy, a symbol of technocratic virtue and collective solidarity. To question them, even mildly, is to associate oneself with populism, or worse, with Trumpism. The press, already predisposed to guard the gates of elite consensus, internalizes this taboo.
This is not a plea for anti-vaccine journalism. It is a plea for symmetry. The same epistemic humility that guides our analysis of finasteride should guide our analysis of immunization. The same willingness to highlight trial flaws, marketing tactics, and adverse effects should apply regardless of whether the product is elective or mandated, aesthetic or immunological.
Finasteride was given to men who wanted hair. Some of them lost more than they bargained for. The Journal’s podcast gave those men a voice. It asked hard questions. It followed the evidence. That same method—scrupulous, skeptical, transparent—should be applied to vaccines. For if journalism is to serve the public, it must ask not merely what is true, but what is allowed to be said.
The answer, increasingly, is that some truths are less equal than others.
If you don't already please follow @amuse on 𝕏.